
Mental Health for the Young & their Families in Victoria is a collaborative partnership between mental health & other health professionals, service users & the general public.
Mailing Address
MHYFVic
PO Box 206,
Parkville, Vic 3052
PROJECT EVIDENCE for Treatment of Mental Disorders. The project coordinator is Dr Allan Mawdsley. The version can be amended by consent. If you wish to contribute to the project, please email admin@mhyfvic.org
[6] Standard Treatment
a) Outpatient psychotherapies, medication and procedures
b) Inpatient psychotherapies, medication and procedures
c) Ancillary support services
[6 a ] Outpatient psychotherapies, medication and procedures
Specialist mental health services should offer a range of therapeutic programs for disabling mental health problems in the community. Service provision, clinical research and training are closely linked in the Tier Three facilities but the practice guidelines published by those services should be implemented at all levels of their service delivery facilities.
These are grouped under nine headings: (i) organic brain disorders, (ii) substance abuse disorders, (iii) psychotic disorders, (iv) mood disorders, (v) anxiety disorders, including stress-related, somatoform and obsessive-compulsive disorders, (vi) physiological disorders, including eating, sleeping and sexual, (vii) personality disorders, (viii) intellectual disability and developmental disorders including autism spectrum disorders, (ix) behavioural and relationship disorders of childhood.
All disorders in childhood require wholistic management involving caregivers. See PE4 for a general outline of case identification and assessment and PE2a(i) for infant mental health. See PE6a(ix) for a general outline of case management for young people.
PE6a (vi) Physiological disorders
This section includes functional problems of bodily systems:
Eating Disorders
Eating disorders are characterised by disturbances of eating behaviours and a core psychopathology centred on food, eating and body image concerns. Eating disorders are associated with notable quality of life impairment and impact on home, work, personal, and social life. Eating disorders also frequently co-occur with other mental health disorders, particularly anxiety disorders and depression.
PHYSICAL WARNING SIGNS INCLUDE:
PSYCHOLOGICAL WARNING SIGNS INCLUDE:
BEHAVIOURAL WARNING SIGNS INCLUDE:
Several variants are described:
Anorexia nervosa was described first in 19th century medical reports, to include self-imposed or maintained weight loss such that the person is underweight (for age and height) and associated overvaluation of shape and weight. This condition is characterised by intense fear of gaining weight/ becoming fat or persistent behaviour that interferes with weight gain. In addition, there is a disturbance in body image and /or undue influence of body weight or shape on self-evaluation and/or persistent lack of recognition of the seriousness of the low body weight.
Two subtypes of anorexia nervosa are specified: restrictive type (with or without compulsive exercise); and binge eating/purging type, with binge eating (uncontrolled overeating) and purging (vomiting, laxative or diuretic misuse).
Bulimia nervosa and binge eating disorder were not described until the 20th century. Bulimia nervosa and binge eating disorder are both defined by having regular and recurrent sustained binge eating episodes. The amount of food eaten is larger than what most people would eat in a similar time period under similar circumstances. There is also a sense of lack of control of overeating during the episode.
People with bulimia nervosa also compensate for binge eating with regular extreme weight control behaviours (such as purging). As they do not engage in such compensation regularly, people with binge eating disorder are likely to be overweight or obese. Self-evaluation is unduly influenced by body shape and weight and the binge eating and inappropriate compensatory behaviours both occur weekly or more frequently over a period of three months. Anorexia nervosa is not present in this condition. The bingeing and purging occur in cycles.
Binge eating disorder in the absence of recurrent inappropriate compensatory behaviours is associated with three or more of the following:
Marked distress regarding binge eating is present and the binge eating occurs at least weekly for three months or more.
Other specified feeding and eating disorder Symptoms characteristic of an eating disorder predominate, cause clinically significant distress or impairment but do not meet the criteria for diagnosis of a disorder in the eating disorders diagnostic category. This may include atypical anxiety nervosa where there is normal weight, low level bulimia nervosa (frequency / duration). Binge eating disorder (low level/limited duration), purging disorder and night eating syndrome.
Orthorexia This refers to an obsession with healthy food, where there is fixation on quality rather than quantity of food to an excessive degree. This can start with ‘healthy” eating and progress to elimination of whole food groups.
Avoidant restrictive food intake disorder (ARFID) which, like binge eating disorder, and in contrast to anorexia nervosa and bulimia nervosa, is not characterised by body image disturbance.
WITHOUT TREATMENT, EATING DISORDERS MAY RESULT IN:
EVIDENCE BASED TREATMENTS:
TREATMENT REFRRALS: PUBLIC/COMMUNITY
REFERRALS PRIVATE SECTOR (FEE FOR SERVICE)
A recommended reference for this topic is provided by the Royal Australian & New Zealand College of Psychiatrists clinical practice guidelines for the treatment of eating disorders Aust NZ J Psychiatry 2014 4:48:977.
Other information came from Eating Disorders Victoria. This group offers telehealth nurse, peer mentoring program, psychology and dietetics, education, primary health, support groups and stories of recovery.
Sleep disorders
Current sleep medicine conceptualizes sleep not as a simple absence of wakefulness and perception or a suspension of sensorial processes but the result of a combination of a passive withdrawal of afferent stimuli to the brain and functional activation of certain neurons in specific brain areas. As such, sleep is considered an active rather than a passive process.
Based on EEG, EMG and electro-oculography patterns, four types (or stages) of sleep can be identified. In an individual without sleep abnormalities, non-rapid eye movement (NREM) and rapid eye movement (REM) phases alternate in a cyclic manner, each cycle lasting on average from 90 to 110 minutes.
In general, sleep requirements decrease from the newborn (about 16 h/day of sleep) to the young child (3-5 years old: 11 h/day), to the older child (10-11 years old: 10 h/day), to the adult (7.5-8 h/day). Sleep cycles last about 45 minutes in young children, 60 minutes in 9-year-olds, and 90-110 minutes after the age of 10 (as in adults).
Recommendations for healthy sleep usually include guidance across a wide range of activities such as adoption of a bedtime routine, consistent bedtime and wake time, a quiet, dark and cool bedroom, avoidance of caffeinated products, and daily physical activities. Healthy sleep practices are also a fundamental component of sleep education designed to prevent sleep problems from developing (primary prevention), to address poor sleep quality (secondary prevention), and to treat existing sleep disorders.
Healthy sleep practices are potential mediating factors between biological sleep needs and environmental circumstances which facilitate or impede sleep. For example, one of the most important elements of a healthy sleep practice is a regular sleep and wake schedule. A consistent bedtime and wake time helps to reinforce circadian rhythms and optimize the sleep drive, processes which are instrumental in regulating healthy sleep-wake cycles.
Another important aspect of healthy sleep practices involves ensuring adequate opportunity for sleep. While there is some variability in sleep needs across individuals, guidelines exist for recommended sleep amounts in children across different ages. When assessing individual sleep needs, it is important to also educate parents about clues which suggest that a child is not getting sufficient sleep (e.g., the child is difficult to wake in the morning or dozes off during the day).
The assessment of sleep and sleep disturbances in children (as well as in adults) is performed by means of subjective (i.e., based on reports by the child and/or parents, +/- rating scales) or, when needed, objective tools (i.e., neurophysiological tests such as polysomnography or infrared video). The latter are undertaken by specialist sleep disturbance programs in paediatric settings.
The main sleep/wake disorders identified are:
Insomnia is “a persistent difficulty with sleep initiation, duration, consolidation, or quality that occurs despite adequate opportunity and circumstances for sleep, and results in some form of daytime impairment” (American Academy of Sleep Medicine, 2014).
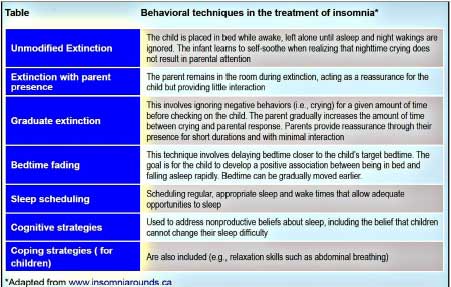
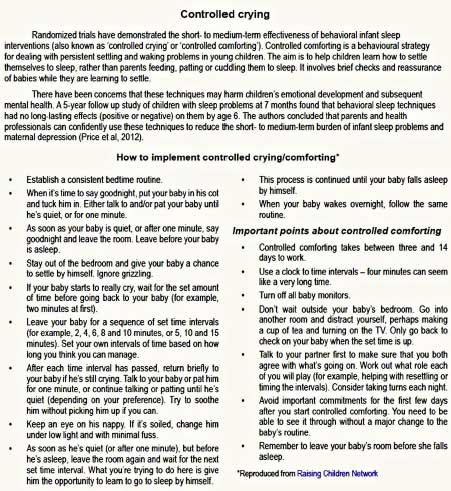
Good sleep practices (see above) and behavioral interventions such as extinction or bedtime fading (see Table below) are the first recommended treatments for pediatric insomnia. Caregivers play a key role in establishing and maintaining normal children’s sleep. Therefore, it is important to discuss parents’ knowledge and beliefs as well as strategies they have used to help address their child’s sleep problems. Providing parents with accurate information about children’s sleep is an essential component of behavioral sleep interventions.
Behavioral strategies should be adapted to the child’s age and to the family’s situation (co-sleeping, shared rooms, etc.). Graduate extinction techniques and controlled crying are more appropriate for younger children, whereas cognitive and coping strategies are better suited to school-aged children. See Table for controlled crying/comforting techniques.
Reference
Cortese S, Ivanenko A, Ramtekkar U & Angriman M. Sleep disorders in children and adolescents: A practical guide. In Rey JM (ed), IACAPAP e-Textbook of Child and Adolescent Mental Health. Geneva: International Association for Child and Adolescent Psychiatry and Allied Professions 2014
Toileting Disorders
Enuresis
nocturnal enuresis denotes an intermittent (i.e., not continuous) wetting during sleep in children after their fifth birthday. It is involuntary (or even intentional) wetting in children, after organic causes have been ruled out. The wetting must have persisted for at least three months to be considered a disorder.
Daytime wetting is termed urinary incontinence, which can be organic (structural, neurogenic or due to other physical causes) or functional.
Enuresis is 2-3 times more common than daytime urinary incontinence; it is 1½ to 2 times more common in boys than girls. Prevalence of night wetting decreases with increasing age: 20% in 4 year-olds, 10% in 7 year-olds, 1%-2% in adolescents, and 0.3%-1.7% among adults.
Enuresis is a genetically determined maturational disorder of the central nervous system; 70% to 80% of all children with enuresis have affected relatives. Genetic and neurobiological factors interact with environmental influences in the pathogenesis of elimination disorders. Genetic factors play a role in daytime urinary incontinence as well.
Psychosocial factors modulate genetic and neurobiological risks in different ways. They play little role in the maturational type where there has never been a dry period but are significant in children whose enuresis begins after having previously achieved dryness (secondary enuresis). Children with secondary enuresis have both higher rates of emotional and behavioural disorders as well as stressful life events prior to the relapse. The age of school entry (5-6 years) is the most common age for relapse while parental separation or divorce is the most important life event.
Enuresis is associated with emotional distress in both children and parents, which is reversible once children become dry. Achieving continence is therefore the main goal of treatment and will lead to an improvement of self-worth and self-confidence. On the other hand, 20%-40% of all children with enuresis have additional, comorbid psychological disorders, not only externalising conditions such as attention deficit hyperactivity disorder (ADHD) and oppositional defiant disorder (ODD) but also internalising disorders such as depression.
These comorbid conditions require separate assessment and treatment –in addition to the symptom-oriented treatment of the child’s elimination disorder.
Assessment and a careful diagnosis are the bases for successful treatment – each subtype of enuresis and urinary incontinence responds best to its specific treatment. It is essential that organic causes of incontinence are ruled out. A paediatric and neurological assessment is recommended. At least one urinalysis (with a urine stick) is recommended to be sure that no signs of bacteriuria and manifest urinary tract infection are present.
Treatment should always be symptom-orientated, aimed at achieving continence (i.e., complete dryness). Primary psychotherapy for enuresis is not effective and not indicated. Comorbid disorders should be treated separately according to evidence-based recommendations. When there are several concurrent disorders, encopresis and constipation should be treated first because some children will stop wetting once these problems have been dealt with. Daytime incontinence should be treated first, as many children will stop wetting at night once the daytime problems have been treated.
A baseline period is recommended with a simple observation and recording of wet and dry nights over a period of 4 weeks. Children are asked to draw a symbol for wet and dry nights (clouds and suns, stars, etc.) in a chart and bring it to the next consultation.
Two main interventions are available: alarm treatment and pharmacotherapy. As alarm treatment is more effective and has the best long-term results, this should be the first line treatment if child and parent are motivated.
An alarm consists of a pad or a metal sensor, which is connected to a bell by a wire. Once the sensor becomes wet, an electric circuit is closed and the alarm is set off. Alarms are very simple devices; they can be cleaned and used by different children many times over.
Children should feel responsible for their treatment. Some instructions are extremely important and should be gone through in detail with parents and child:
Some children become dry in only a few weeks, most will require 8 to 10 weeks and some a little longer. After 14 consecutive dry nights, use of the alarm is discontinued and the child is considered to be dry. Parents are advised to restart alarm treatment if a relapse (two wet nights per week) happens. The alarm treatment relies on operant conditioning and should be enhanced with other measures including positive reinforcement with praise and other rewards, as well as aversive consequences such as getting up, going to the toilet and remaking the bed.
Indications for medication are:
There are two groups of medication with a clear antienuretic effect – desmopressin and tricyclic antidepressants (TCAs). Although both are effective, desmopressin has less side-effects and is therefore the preferred substance.
Desmopressin (1-deamino-8-D-arginine vasopressin, abbreviated DDAVP) is a synthetic analogue of the antidiuretic hormone (ADH). A reduction of wet nights or even dryness can be achieved in 70% of cases: 30% of children are full responders, 40% partial responders, and 30% non-responders. However, after discontinuing medication most children relapse.
Enuresis has excellent long-term outcome with a high spontaneous remission rate – 13% per year – and effective treatments are available; 60% to 80% become dry with alarm treatment and 50% remain so on the long-term.
Reference
von Gontard A. Enuresis. In Rey JM (ed), IACAPAP e-Textbook of Child and Adolescent Mental Health. Geneva: International Association for Child and Adolescent Psychiatry and Allied Professions 2012.
Encopresis
Encopresis is defined as both voluntary and involuntary passage of faeces in inappropriate places in a child aged four years or older, after organic causes have been ruled out. Two major forms of encopresis can be differentiated: encopresis with and without constipation. The specific differentiation into these two subtypes is of utmost importance as they differ according to pathophysiology, clinical features and, especially, treatment.
Three to four times more boys are affected by encopresis than girls. Encopresis occurs almost always during the day. Nocturnal encopresis is more often associated with organic causes and requires a more detailed somatic assessment.
Children with encopresis with constipation have a reduced number of bowel movements with large stools of altered consistency (too soft or too hard). They often experience pain during defecation. Abdominal pain and reduced appetite are typical. The colon transit time is increased, abdominal and rectal masses are palpable. In sonography, the rectal diameter is increased (> 25 mm). Often, daytime urinary incontinence and even enuresis co-exists. Additional emotional and behavioral disorders are found in 30%-50% of them and, finally, laxative therapy is helpful.
Children with encopresis without constipation do not have many of these symptoms. They have daily bowel movements of normal size and consistency. Pain is not frequent and appetite is good. Colon transit time is normal and no stool masses can be palpated. Enuresis and urinary incontinence are less common, while comorbidity with psychological disturbances is similar (30%-50%). Finally, laxatives have no effect – can even worsen the soiling.
In contrast to the type with constipation, the etiology of this type is uncertain. The comorbidity rate of both types of encopresis is similar: 30%-50% of cases. This means, that three to five times more children with encopresis have additional disturbances in comparison to non-soiling children, but these disturbances are diverse.
The psychoanalytic construct of anal-retentive personality traits associated with parent-child power struggles is sometimes seen and can be a useful guide to engaging the child at winning control of his toileting rather than the battle to hide his soiling from disapproving adults.
Assessment
The assessment of children with encopresis should be as non-invasive as possible and should always include parents or other caregivers. For most children, a basic evaluation that can be conducted in many primary care settings is sufficient. If conducted correctly and empathically, the most relevant information will be gathered through the history.
A very useful chart is the Bristol Stool Chart. Seven types of stool forms are depicted ranging from “separate hard lumps, like nuts (hard to pass)” (type 1) to “watery, no solid pieces, entirely liquid” (type 7). The scale enables parents and children to identify the predominant type of stool easily and without lengthy descriptions. The course of treatment can also be monitored using this scale.
Each child should have a physical examination. If sonography is available, this can replace the rectal exam if no organic form or fecal incontinence is suspected. Other examinations are not routinely indicated – only if an organic type of fecal incontinence is suspected. It is important to avoid unnecessary and invasive investigations. Somatic causes are present in only 5% of children with chronic constipation, and 1% of children without, but must be ruled out.
Treatment
Following assessment, children and parents are given detailed information on the subtype of encopresis. High fibre diet with ample fluids is recommended. Toilet training is initiated right from the start for both types of encopresis. A useful booklet for child and parents is “Beating Sneaky Poo”, which can be viewed on the ‘Library Resources’ page of this website.
(a) For encopresis with constipation.
In children with constipation, toilet training is combined with laxatives: first disimpaction, then maintenance treatment. Disimpaction is necessary to evacuate fecal masses at the beginning of treatment. This can be performed rectally or orally. In rectal disimpaction, enemas are applied. An alternative is oral disimpaction with polyethylenglykol. Sufficient oral fluids are required for this osmotic laxative to be effective.
(b) For encopresis without constipation.
Toilet training is the main aspect of treatment, combined with psychotherapy. Laxatives are not indicated.
Toilet training
An essential pre-requisite is engagement of the child in taking responsibility for his participation. The aim of training is to establish a regular daily toileting routine. (Most children from the age of four years onwards have one bowel movement a day but may not have established their own routine.)
If the child has a preferred time it should be chosen for the routine, otherwise try to engage the child in finding the time he likes best. (Morning before leaving for school is generally the most effective).
The child is asked to sit on the toilet three times a day, after mealtimes.
This time is especially useful as the postprandial defecation reflexes are then most active. Children are asked to sit on the toilet five to ten minutes in a relaxed way. For this, to minimise apprehensiveness it is important that their feet touch the floor. Otherwise, a little foot-stool should be provided.
These toilet sessions should be experienced in a positive way: children are allowed to read comics, books, play with computers or cell phones, draw pictures, etc. They are not expected to pass urine or stools every time.
These toilet sessions are documented in a chart to show participation and productivity. If necessary, the co-operation of the child can be enhanced positively by a simple token system with small rewards. The reward is for participation in the attempt, not for its production. All criticism or punishment should be avoided.
Discussion with the child about progress may establish a preferred time that enables the routine to be reduced to once daily at that time. This supports the child’s ownership of the decision and likelihood of success.
If comorbid emotional and behavioral disorders are present, these need to be treated separately. Untreated comorbid disorders will reduce adherence and compliance and outcome of encopresis treatment will not be optimal.
Reference
von Gontard A. Encopresis. In Rey JM (ed), IACAPAP e-Textbook of Child and Adolescent Mental Health. Geneva: International Association for Child and Adolescent Psychiatry and Allied Professions 2012.
Heins,T. and Ritchie,K.”Beating Sneaky Poo: Ideas for faecal soiling” Second edition, 1988. Accessed from https://dulwichcentre.com.au/beating-sneaky-poo-2.pdf also in Library Resources of this website.
Sexual Disorders
Sexual attraction or sexual orientation is a separate concept from gender identity. Sexual orientation refers to the type of individuals toward whom one is romantically or sexually attracted. Terms such as androphilia (attraction to males), gynephilia (attraction to females), biphilia (attraction to males and females), and aphilia (attraction to neither males nor females) have become more common, slowly replacing older terms such as heterosexual, bisexual, homosexual, and asexual.
The consensus of scientific research and clinical literature demonstrate that same-sex attractions, feelings, and behaviours are normal and positive variations of human sexuality. There is now a large body of scientific evidence that indicates that being gay, lesbian or bisexual is compatible with normal mental health and social adjustment.
The American Psychiatric Association and the American Psychological Association, in recognition of scientific evidence, removed homosexuality from the lexicon and called on all mental health professionals to take the lead in “removing the stigma of mental illness that has long been associated” with homosexuality.
The vast majority of newborns are assigned the gender of boy or girl through prenatal diagnostics or, at birth, based on genital anatomy. A small number of newborns may be classified as having a “disorder of sex development” or congenital conditions in which biological parameters of sex (e.g., the sex chromosomes, the gonads, the configuration of the external genitalia, etc.) are incongruent with one another. Such patients may experience gender identity issues different from those experienced by individuals without a disorder of sex development.
Experienced gender or gender identity refers to one’s sense of self as a boy, as a girl, or some alternative gender that is different from the traditional boy-girl dichotomy. Gender, being a core feature of identity, is influenced by the language spoken. In some languages the words for sex and gender are the same. This may make it harder to differentiate between gender identity versus anatomical sex.
Current diagnostic criteria for gender dysphoria in children require a marked incongruence between one’s experienced/expressed gender and assigned gender, of at least six months’ duration, as evidenced by at least six of eight criteria, one of which must be a strong desire to be of the other gender or an insistence that one is the other gender (or some alternative gender different from one’s assigned gender). Additionally, the patient must experience clinically significant distress or impairment in social, school, or other important areas of functioning.
Etiological evidence suggests that both psychosocial and biological elements are involved. A single mechanism is unlikely and gender dysphoria most likely results from a complex interaction between these factors. Children and adolescents with gender incongruence exhibit higher internalizing and externalizing psychopathology compared to non-referred controls, with internalizing psychopathology being more common, particularly in birth-assigned boys.
These individuals are subjected to rates of peer bullying as high as 80%. Self-harming and suicide attempts are very prevalent among gender nonconforming youth. Gender clinics report high rates of past suicide attempts by patients presenting for care. A number of studies show that autism spectrum disorder (ASD) symptoms are over-represented among transgender individuals.
Assessment
Working with children and youth presenting with gender issues requires knowledge of the child’s psychosexual development, cultural aspects of gender and its expression in that specific society and family unit, as well as their exposure and understanding of the expanding information and media awareness around gender non-conformity and transgender identity.
In the case of working with immigrant families, understanding the interaction of the host and home cultures is also important. Assessment of youth presenting with gender-related concerns requires a developmental history that explores general psychological development, gender development, and a careful analysis of the child’s environment and safety related to expressed gender non-conforming behaviors. Various developmental theories may provide assistance in understanding and categorizing children based on their age in regard to gender development.
Gender dysphoria is a clinical diagnosis and requires in depth and longitudinal evaluation of these youth. The evaluation of gender, in addition to the usual developmental and mental health evaluation of a child, needs to include a thorough chronological history of the child’s gender expression and identity from parents and caregivers as well as a developmentally informed evaluation of the child’s gender individually.
The evaluator may use tools such as toys, books, drawing or playing materials to assist in the evaluation and gather information about behavior at school, with peers and at home. Several scales have also been developed to help with the assessment of gender nonconforming youth (The Utrecht Gender Dysphoria Scale, The Gender Identity/Gender Dysphoria Questionnaire for Adolescents and Adults, among others), though none of these alone can establish a diagnosis.
Families play a key role in the evaluation. A child’s gender variance has a significant impact on the family dynamics and may lead to conflicts and disruption of emotional attachments. It is important that these issues be identified and efforts be made to include all parties involved in the child’s life regardless of the child’s age.
Safety is a complex matter in the lives of gender non-conforming and transgender youth. Mental health practitioners need to be aware and look for overt and covert aggression and risk to the child due to being a sexual and gender minority, in addition to the usual safety issues. Bullying, risk of being kicked out of home, societal violence, and local legislation prosecuting or endangering a youth need to be considered and documented.
Treatment
Three philosophies of treatment are seen at present:
Promoting Identification with the Gender Assigned at Birth
This approach aims to reduce, through psychosocial interventions, the child’s cross-gender identification and gender dysphoria. These treatments assume that gender identity is not yet fixed in childhood and may be malleable through psychosocial treatment. There is also an implicit assumption that all things considered, a child’s long-term adaptation might be easier if he or she could come to feel content with a gender identity that matches their natal sex.
Watchful Waiting
The second approach takes an intermediate therapeutic position. On the one hand, it does not recommend an early gender social transition because children with gender dysphoria may desist for one reason or another. On the other hand, it does not explicitly recommend any type of limit-setting on the child’s gender variant behavior, with the exception that in certain environments it might be risky or dangerous to display such behavior, the “only at home” rule.
This approach also does not favor one type of long-term outcome over another, noting that it is difficult to predict outcome for an individual child and that the more important focus should be on the child’s general psychosocial adjustment and wellbeing.
Affirmative Approach
The affirmative approach considers all outcomes of gender identity to be equally desirable and affirms any gender identity the child expresses. It theorizes that clinician and parental attempts to push children with gender incongruence to conform with their gender assigned at birth might produce shame and stigma that can ultimately lead to psychopathology.
Though similar to the watchful waiting model, an important difference is in its attitude regarding early social transition. In the affirmative model, prepubertal children who express a desire to socially transition and live full time in their experienced gender (i.e., using cross-gender pronouns, a cross-gender name, crossgender clothing, etc.) are allowed to do so.
The approach to social transition must be carefully individualized with a nuanced understanding of the child’s gender identification and the level of support within the child’s community; there must also be an open discussion with the child highlighting that, despite the social transition, the patient is free to transition back at any time.
Separate from the question of persistence is the question of mental health outcome following social transition. Though early work suggests that socially transitioned children have better mental health metrics than children who did not socially transition, future research is needed to fully understand the dynamic and long-term effects of social transition in a broader population.
Gender nonconforming and gender dysphoric youth represent a vulnerable demographic with high rates of co-occurring psychiatric conditions and suicidal behavior, likely secondary to minority stress and dysphoria related to living in a body that does not match one’s experienced gender.
Prepubescent children with gender variant behavior or identification are best supported with psychotherapy and socio-familial interventions. For those children who continue to have strong cross-sex identification in adolescence, pubertal blockade and cross-sex hormone therapy to align patients’ bodies with their experienced identities have been shown to improve mental health outcomes.
Reference
Turban JL, de Vries ALC, Zucker KJ, Shadianloo S. Transgender and gender non-conforming youth. In Rey JM (ed), IACAPAP e-Textbook of Child and Adolescent Mental Health. Geneva: International Association for Child and Adolescent Psychiatry and Allied Professions 2018.
Attentional Disorders
Attention-Deficit/Hyperactivity Disorder (ADHD) is a neurodevelopmental condition characterized by frequent, pervasive and impairing inattention and/or hyperactivity/impulsivity. Studies indicate a prevalence of about 1:14 in Australian children, similar worldwide. Etiology is estimated 70% genetic and 30% environmental.
Environmental risk factors identified in population meta-analyses include:
Prenatal and perinatal factors: low birth weight, prematurity, in-utero exposure to maternal stress, maternal obesity, hypertension, cigarette smoking, alcohol, prescribed drugs (e.g., acetaminophen, valproate), and illicit substances.
Environmental toxins (in-utero or during early childhood): lead, organophosphate pesticides, and polychlorinated biphenyls.
Studies suggest that the neurobiology of ADHD is heterogenous, reflected in the multiple symptoms of the condition. Despite differences from the “typical brain”, these biological markers are not sufficiently sensitive and specific to diagnose the disorder. Similarly, there is no neuropsychological test with sufficient predictive power to diagnose ADHD. The neuropsychological deficits in ADHD emphasize behavioural inhibition, including disruption of working memory, sustained attention, motor control, and affect regulation.
The diagnosis, therefore, is a clinical one. ADHD is defined by the presence of a persistent pattern of inattention and/or hyperactivity-impulsivity that interferes with normal functioning or development. Manifestations of inattention are numerous, including mind wandering while performing a task, lack of persistence, and disorganization.
An important aspect of assessment is to exclude other disorders producing similar attentional problems. These include lead toxicity, frontal lobe impairments from Foetal Alcohol Syndrome or acquired brain injury, also some medical conditions such as thyrotoxicosis, fragile-X syndrome, and psychiatric conditions such as bipolar disorder and generalised anxiety disorder.
The most common comorbid conditions in children are oppositional defiant disorder (ODD), conduct disorder (CD), intellectual disability, learning disorders, language disorders, sleep disorders, enuresis, developmental motor coordination disorders, depressive and anxiety disorders, tic disorders, and autism spectrum disorders.
A meta-analysis found that children with ADHD are 10 times more likely to have CD or ODD, five times more likely to suffer from depression, and three times more likely to have anxiety disorders compared with those without ADHD. There was no significant difference in comorbidity profiles between boys and girls. In adolescents and adults, eating disorders, substance use disorders, bipolar disorder, and personality disorders are also more frequent.
Treatment
There are various treatment strategies that can ameliorate ADHD symptoms which are supported by evidence. Given the variation among patients, an individualized treatment plan is needed, taking into account age, comorbidities, severity, family and social circumstances, and preferences of the patient and family. The patient and family must always be involved in this process.
Because ADHD is a chronic, potentially lifelong condition, psychoeducation is the foundation for any treatment. Clinicians should pay attention to giving information in a way that families can understand, using language, comparisons, and metaphors at the patient educational level and in a culturally sensitive manner. This would include:
Behavioural interventions are indicated as the first line of treatment mainly for younger children and for those who have mild symptoms and impairment. Other psychological approaches used for treating ADHD include behaviour classroom interventions, social and organizational skills training, meditation-based therapy, and cognitive therapy.
Psychostimulants—methylphenidate and amphetamines—are the most studied drugs for ADHD and among the best researched in psychiatry. Methylphenidate is the most widely available. They have the limitation of a short half-life, thus requiring two or three doses during the day for optimal benefit—creating considerable practical problems particularly at school.
Although more potent than methylphenidate, the amphetamines are less often used due to unwarranted concerns about potential for abuse (the dosage for abuse being 20+ times greater than clinical dose).
Specific disorders such as depression and bipolar disorder may present with or exacerbate ADHD symptoms. In these cases, the best course of action may be to treat the comorbid disorder first; the clinician can then assess the ADHD by focusing on the remaining symptoms.
Reference
de Freitas de Sousa A, Coimbra I M, Castanho J M, Polanczyk GV, Rohde LA. Attention deficit hyperactivity disorder. In Rey JM & Martin A (eds), JM Rey’s IACAPAP e-Textbook of Child and Adolescent Mental Health. Geneva: International Association for Child and Adolescent Psychiatry and Allied Professions 2020.
Motor Disorders
Tic disorder
Tics are sudden, rapid, recurrent, nonrhythmic motor movements or vocalisations. Motor tics range from simple, hardly noticeable flinching of the eye to a painful, socially incapacitating and subjectively shameful phenomena involving several muscle groups, for example crouching down or hopping. Vocal or phonic tics are involuntary utterances of sounds, noises, sentences or words.
A simple vocal tic may be a slight coughing, clearing of throat, wheezing, squeaking or loud shouting. More complex vocal tics involve syllables, words or sentences. Coprolalia is the utterance of obscene or aggressive words or sentences. Coprolalia occurs seldom, in less than 20%.
Those afflicted by tics, as well as their family, may experience substantial suffering due to the symptoms, be it through bullying or to inappropriate response by caregivers resulting in a dysfunctional parent-child relationship.
People in the extended environment may also react with irritation, for instance where vocal tics occur in inappropriate settings, such as the cinema or the classroom. On the other hand, some of the people afflicted successfully develop strategies to control their tics and learn to live and cope with them.
It is estimated that 4% to12 % of all children suffer from tics at some time during their development. Approximately 3%-4% are afflicted by a chronic tic disorder and 1% with Tourette’s syndrome. Children and adolescents are 10 times more likely to suffer from tics than adults. This may be due to the high spontaneous remission rate in younger patients.
Boys are afflicted three to four times more often than girls. A familial predisposition has been established Transient tic disorders (less than 12 months duration) mostly occur in school age children and usually do not require specific treatment.
Diagnosis of Gilles-de-la-Tourette syndrome (or simply Tourette syndrome or disorder) is warranted in cases where several motor tics and at least one vocal tic are present at the same time or have been present in the past. Motor and vocal tics do not have to be present at the same time but should have occurred almost every day over one year at least to warrant the diagnosis. The onset of Tourette syndrome is generally before the age of 18.
Although the cause of primary tic disorders has not been conclusively determined, it is widely assumed to be the result of an interaction of genetic, neurobiological and psychological factors as well as environmental influences. Heritability has been estimated to be around 50 %. Around 90% of those with TS develop one or more psychiatric disorders. The probability of having a comorbid disorder increases with the severity of tics, early onset and familial loading.
The clinical assessment (see PE4) should include a thorough physical and neurological examination, including an EEG. The main purpose for this is to exclude other possible illnesses that could cause the symptoms.
Psychoeducation involves providing detailed information to the relevant persons, in the case of young people this usually will involve parents and teachers. Information should be provided regarding the disorder, its course, investigations and options for treatment. Information which often is of use to teachers involves recommending allowing the child to sit exams on their own or to be permitted to leave the classroom for short periods – to lessen the urge to release the tics.
Cognitive behavioural methods are the most effective psychotherapeutic intervention. This treatment should be administered by trained professionals well versed in the complexities of the disorder. It may involve the following:
Medication
Reference
Metzger H, Wanderer S, Veit Roessner V. Tic disorders. In Rey JM (ed), IACAPAP e-Textbook of Child and Adolescent Mental Health. Geneva: International Association for Child and Adolescent Psychiatry and Allied Professions 2012.
Stuttering
Stuttering is a clinical syndrome involving abnormal and persistent dysfluencies that result in the speaker’s perception of a loss of control over speech, which is often accompanied by affective and behavioural reactions. Several types of speech dysfluencies also may be involved, including blocking of sounds, hesitations, and tense pauses. Stuttering usually begins somewhere between 2 and 7 years of age, with a peak between 3 and 4 years.
Although normal children often go through periods of dysfluency during the developmental period, these “normal dysfluencies” tend to occur in the larger linguistic units (word, phrases, and sentences). For children who tend to persist in stuttering over time, dysfluencies are more likely to occur in repetitions of syllables and sounds.
Other “red flags” for persistent stuttering include sound prolongations, silent blocks in which the child attempts to speak but no sound comes out, and visible struggle behaviours during speech, such as blinks or grimaces. If dysfluencies continue to be relatively effortless, there is a good chance of recovery. Children who recover from stuttering begin to show reductions in their number of dysfluencies within the first year, whereas those who persist in stuttering are relatively stable in their rate of dysfluency.
When recovery occurs, it usually does so by adolescence, often around the time of puberty. About 1 in 30 children goes through a period of stuttering, but by adolescence, the prevalence drops to 0.8%. The disorder is much more common in boys than in girls, and the male/female ratio increases with age, suggesting that girls show higher rates of recovery than boys.
For individuals with chronic stuttering, the severity of the disturbance varies from situation to situation and is more severe when there is pressure to communicate. Stress or anxiety have been shown to exacerbate stuttering, but are not thought to play a role in the etiology. Reducing stress during speaking can reduce stuttering episodes, but general treatments for anxiety, including the use of tranquilizing medication, have not been found to be effective treatments.
ln general, speech therapy is used both to shape fluent speech and help the client to stutter with less tension, avoidance, and interruption of the flow of communication. Psychotherapy alone has not been shown to be an effective treatment for stuttering, but counselling is often helpful for overcoming the secondary effects of stuttering on self-concept, thoughts, and feelings.
Although stuttering has, at times, been thought to be a learned behaviour, most researchers today consider stuttering to have a biological component. People who stutter have been found to show laryngeal behaviour different from that in normal speakers, even when their speech is apparently fluent. Elements of both the central and peripheral nervous system may be involved in stuttering behaviours.
There also appears to be a familial component in stuttering. The risk of stuttering among first-degree relatives is more than three times the population risk. Stuttering is believed by most researchers today to have a complex multiplicity of causes that include biological vulnerability, environmental demands and expectations, and temperamental characteristics of the speaker.
Reference
Paul,R. “Disorders of communication” in Lewis,M. Child and Adolescent Psychiatry, 3rd edition, 2002, Lippincott Williams & Wilkins.
Last updated 10/1/2022
POLICIES for Treatment of Mental Disorders. The project coordinator is Dr Allan Mawdsley. The version can be amended by consent. If you wish to contribute to the project, please email admin@mhyfvic.org
[6] Standard Treatment
a) Outpatient psychotherapies, medication and procedures
b) Inpatient psychotherapies, medication and procedures
c) Ancillary support services
[6 a ] Outpatient psychotherapies, medication and procedures
MHYFVic advocates that Specialist mental health services should offer a range of therapeutic programs for disabling mental health problems in the community. All disorders in childhood require wholistic management involving caregivers.
Service provision, clinical research and training should be integrated in the Tier Three facilities, with the practice guidelines published by those services implemented at all levels of their service delivery facilities. The baseline standard of case assessment required is that outlined in PE4 (and PE2a(i) for infant mental health)
POL6a (vi) Physiological Disorders
MHYFVic advocates that Specialist mental health services should offer multidisciplinary assessment and treatment programs for children with physiological disorders including:
Last updated 9/2/2022
PROJECT EVIDENCE for Treatment of Mental Disorders. The project coordinator is Dr Allan Mawdsley. The version can be amended by consent. If you wish to contribute to the project, please email admin@mhyfvic.org
[6] Standard Treatment
a) Outpatient psychotherapies, medication and procedures
b) Inpatient psychotherapies, medication and procedures
c) Ancillary support services
[6 a ] Outpatient psychotherapies, medication and procedures
All disorders in childhood require wholistic management involving caregivers. See PE4 for a general outline of case identification and assessment and PE2a(i) for infant mental health. See PE6a(ix) for a general outline of case management for young people.
BP6a (vi) Physiological Disorders
The general principles of clinical assessment and case planning mentioned in the preceding paragraph are modified in each of the subgroupings because of the need for specialist expertise in the management of specific disorders. This is described in the Project Evidence subsections.
The subsections are:
EATING DISORDERS
EVIDENCE BASED TREATMENTS:
TREATMENT REFERRALS: PUBLIC/COMMUNITY
REFERRALS PRIVATE SECTOR (FEE FOR SERVICE)
A recommended reference for this topic is provided by the Royal Australian & New Zealand College of Psychiatrists clinical practice guidelines for the treatment of eating disorders Aust NZ J Psychiatry 2014 4:48:977.
Other information came from Eating Disorders Victoria. This group offers telehealth nurse, peer mentoring program, psychology and dietetics, education, primary health, support groups and stories of recovery.
SLEEP DISORDERS
Recommendations for healthy sleep usually include guidance across a wide range of activities such as adoption of a bedtime routine, consistent bedtime and wake time, a quiet, dark and cool bedroom, avoidance of caffeinated products, and daily physical activities. Healthy sleep practices are also a fundamental component of sleep education designed to prevent sleep problems from developing (primary prevention), to address poor sleep quality (secondary prevention), and to treat existing sleep disorders.
Healthy sleep practices are potential mediating factors between biological sleep needs and environmental circumstances which facilitate or impede sleep. For example, one of the most important elements of a healthy sleep practice is a regular sleep and wake schedule. A consistent bedtime and wake time helps to reinforce circadian rhythms and optimize the sleep drive, processes which are instrumental in regulating healthy sleep-wake cycles.
Another important aspect of healthy sleep practices involves ensuring adequate opportunity for sleep. While there is some variability in sleep needs across individuals, guidelines exist for recommended sleep amounts in children across different ages. When assessing individual sleep needs, it is important to also educate parents about clues which suggest that a child is not getting sufficient sleep (e.g., the child is difficult to wake in the morning or dozes off during the day).
The assessment of sleep and sleep disturbances in children (as well as in adults) is performed by means of subjective (i.e., based on reports by the child and/or parents, +/- rating scales) or, when needed, objective tools (i.e., neurophysiological tests such as polysomnography or infrared video). The latter are undertaken by specialist sleep disturbance programs in paediatric settings.
TOILETING DISORDERS
Enuresis
Assessment and a careful diagnosis are the bases for successful treatment – each subtype of enuresis and urinary incontinence responds best to its specific treatment. It is essential that organic causes of incontinence are ruled out. A paediatric and neurological assessment is recommended. At least one urinalysis (with a urine stick) is recommended to be sure that no signs of bacteriuria and manifest urinary tract infection are present.
Treatment should always be symptom-orientated, aimed at achieving continence (i.e., complete dryness). Primary psychotherapy for enuresis is not effective and not indicated. Comorbid disorders should be treated separately according to evidence-based recommendations.
When there are several concurrent disorders, encopresis and constipation should be treated first because some children will stop wetting once these problems have been dealt with. Daytime incontinence should be treated first, as many children will stop wetting at night once the daytime problems have been treated.
A baseline period is recommended with a simple observation and recording of wet and dry nights over a period of 4 weeks. Children are asked to draw a symbol for wet and dry nights (clouds and suns, stars, etc.) in a chart and bring it to the next consultation.
Two main interventions are available: alarm treatment and pharmacotherapy. As alarm treatment is more effective and has the best long-term results, this should be the first line treatment if child and parent are motivated.
Encopresis
The assessment of children with encopresis should be as non-invasive as possible and should always include parents or other caregivers. For most children, a basic evaluation that can be conducted in many primary care settings is sufficient. If conducted correctly and empathically, the most relevant information will be gathered through the history.
A very useful chart is the Bristol Stool Chart. Seven types of stool forms are depicted ranging from “separate hard lumps, like nuts (hard to pass)” (type 1) to “watery, no solid pieces, entirely liquid” (type 7). The scale enables parents and children to identify the predominant type of stool easily and without lengthy descriptions. The course of treatment can also be monitored using this scale.
Each child should have a physical examination. If sonography is available, this can replace the rectal exam if no organic form or fecal incontinence is suspected. Other examinations are not routinely indicated – only if an organic type of fecal incontinence is suspected.
It is important to avoid unnecessary and invasive investigations. Somatic causes are present in only 5% of children with chronic constipation, and 1% of children without, but must be ruled out.
Following assessment, children and parents are given detailed information on the subtype of encopresis. High fibre diet with ample fluids is recommended. Toilet training is initiated right from the start for both types of encopresis. A useful booklet for child and parents is “Beating Sneaky Poo”, which can be viewed on the ‘Library Resources’ page of this website.
(a) For encopresis with constipation.
In children with constipation, toilet training is combined with laxatives: first disimpaction, then maintenance treatment. Disimpaction is necessary to evacuate fecal masses at the beginning of treatment. This can be performed rectally or orally. In rectal disimpaction, enemas are applied. An alternative is oral disimpaction with polyethylenglykol. Sufficient oral fluids are required for this osmotic laxative to be effective.
(b) For encopresis without constipation.
Toilet training is the main aspect of treatment, combined with psychotherapy. Laxatives are not indicated.
SEXUAL DISORDERS
Gender dysphoria is a clinical diagnosis and requires in depth and longitudinal evaluation of these youth. The evaluation of gender, in addition to the usual developmental and mental health evaluation of a child, needs to include a thorough chronological history of the child’s gender expression and identity from parents and caregivers as well as a developmentally informed evaluation of the child’s gender individually.
The evaluator may use tools such as toys, books, drawing or playing materials to assist in the evaluation and gather information about behavior at school, with peers and at home. Several scales have also been developed to help with the assessment of gender nonconforming youth (The Utrecht Gender Dysphoria Scale, The Gender Identity/Gender Dysphoria Questionnaire for Adolescents and Adults, among others), though none of these alone can establish a diagnosis.
Because inferior management can be harmful, it is essential for assessment and management to be undertaken only by reputable specialist services (such as the Royal Children’s Hospital).
ATTENTIONAL DISORDERS
The diagnosis of ADHD is a clinical one, defined by the presence of a persistent pattern of inattention and/or hyperactivity-impulsivity that interferes with normal functioning or development. An important aspect of assessment is to exclude other disorders producing similar attentional problems.
These include lead toxicity, frontal lobe impairments from Foetal Alcohol Syndrome or acquired brain injury, also some medical conditions such as thyrotoxicosis, fragile-X syndrome, and psychiatric conditions such as bipolar disorder and generalised anxiety disorder.
The most common comorbid conditions in children are oppositional defiant disorder (ODD), conduct disorder (CD), intellectual disability, learning disorders, language disorders, sleep disorders, enuresis, developmental motor coordination disorders, depressive and anxiety disorders, tic disorders, and autism spectrum disorders.
Best practice assessment clearly requires both paediatric medical appraisal and psychological appraisal. Equally, case management requires consideration of both domains. Medication alone, without psychological intervention, is malpractice.
MOTOR DISORDERS
Tic Disorders
The clinical assessment (see PE4) should include a thorough physical and neurological examination, including an EEG. The main purpose for this is to exclude other possible illnesses that could cause the symptoms. Psychoeducation involves providing detailed information to the relevant persons, in the case of young people this usually will involve parents and teachers.
Cognitive behavioural methods are the most effective psychotherapeutic intervention. This treatment should be administered by trained professionals well versed in the complexities of the disorder.
Stuttering
Stuttering is a clinical syndrome involving abnormal and persistent dysfluencies that result in the speaker’s perception of a loss of control over speech, which is often accompanied by affective and behavioural reactions. Assessment should be undertaken by a specialist Speech Pathologist.
ln general, speech therapy is used both to shape fluent speech and help the client to stutter with less tension, avoidance, and interruption of the flow of communication. Psychotherapy alone has not been shown to be an effective treatment for stuttering, but counselling is often helpful for overcoming the secondary effects of stuttering on self-concept, thoughts, and feelings.
Last updated 10/2/2022
We welcome discussion about any of the topics in our Roadmap epecially any wish to develop the information or policies.
Please send your comments by email to admin@mhyfvic.org
Speak about issues that concern you such as gaps in services, things that shouldn’t have happened, or things that ought to happen but haven’t; to make a better quality of service…….
Help achieve better access to services & better co-ordination between services together we can…….

Mental Health for the Young & their Families in Victoria is a collaborative partnership between mental health & other health professionals, service users & the general public.
MHYFVic
PO Box 206,
Parkville, Vic 3052

Please fill in the details below and agree to the conditions to apply for MHYFVic membership.