
Mental Health for the Young & their Families in Victoria is a collaborative partnership between mental health & other health professionals, service users & the general public.
Mailing Address
MHYFVic
PO Box 206,
Parkville, Vic 3052
PROJECT EVIDENCE for Treatment of Mental Disorders. The project coordinator is Dr Allan Mawdsley. The version can be amended by consent. If you wish to contribute to the project, please email admin@mhyfvic.org
[6] Standard Treatment
a) Outpatient psychotherapies, medication and procedures
b) Inpatient psychotherapies, medication and procedures
c) Ancillary support services
[6 a ] Outpatient psychotherapies, medication and procedures
Specialist mental health services should offer a range of therapeutic programs for disabling mental health problems in the community. Service provision, clinical research and training are closely linked in the Tier Three facilities but the practice guidelines published by those services should be implemented at all levels of their service delivery facilities.
These are grouped under nine headings: (i) organic brain disorders, (ii) substance abuse disorders, (iii) psychotic disorders, (iv) mood disorders, (v) anxiety disorders, including stress-related, somatoform and obsessive-compulsive disorders, (vi) physiological disorders, including eating, sleeping and sexual, (vii) personality disorders, (viii) intellectual disability and developmental disorders including autism spectrum disorders, (ix) behavioural and relationship disorders of childhood.
All disorders in childhood require wholistic management involving caregivers. See PE4 for a general outline of case identification and assessment and PE2a(i) for infant mental health. See PE6a(ix) for a general outline of case management for young people.
PE6a (viii) Developmental Disorders and Intellectual Disability
Every Human Being is unique but will share many characteristics with other humans. Our diverse range of abilities differs amongst individuals and attempts are made to describe and measure the differences. The descriptions generally consider our abilities in the domains of cognitive, language, motor, and social abilities, notwithstanding that there is considerable overlap across domains.
Observations of development in populations reveal normative patterns and examples outside the typical patterns. Attempts are made to measure the degrees of abilities by construction of normative tests, which are generally useful although always merely approximations of the actual abilities. High levels of abilities are generally valued whereas low levels are generally called disabilities.
Scientific studies of the biological, psychological and social factors underpinning development attempt to define the reasons for disabilities (the etiology). This can open the way to prevent or ameliorate disabilities. Scientific study not only attempts to find the etiological disorder and define the degree of disability or impairment but also to avoid social factors that make the disability a handicap in daily life.
When a child’s developmental progress is suspected of being outside the normal range, a careful clinical assessment should be undertaken.
This is described in PE4 (Case identification). The generic assessment approach is modified by the addition of specific elements as the nature of the underlying disorder is clarified. It is not the purpose of this paper to separately consider each of the vast number of different disabilities, but in outlining some general principles will use two commonly encountered examples as a platform for approach. These are 1) Intellectual Disability as an example of global impairment, and 2) autism spectrum disorder as an example of a more focal impairment.
INTELLECTUAL DISABILITY
The term ‘intellectual disability’ (ID) is defined as “a condition of arrested or incomplete development of the mind, which is especially characterized by impairment of skills manifested during the developmental period, which contribute to the overall level of intelligence, i.e., cognitive, language, motor, and social abilities.” (World Health Organization, WHO, 1992).
The etiology of ID is heterogeneous. Injury, infections and toxins have become less prevalent causes because of improved antenatal care, while genetic factors have become more prominent. No specific etiology can be found in up to 40% of cases, particularly in mild ID. Environmental influences (e.g., malnutrition, emotional and social deprivation experienced, for example, in poorly run orphanages) can also cause or aggravate ID.
Currently the test results are standardised against a representative sample of the population; IQ scores for children are relative to children of the same age. The median result is defined to be 100 and one standard deviation is 15 points, therefore, 95% of the population have scores within two standard deviations of the mean (i.e., within an IQ range of 70 to 130).
For IQ to be accurate it needs to be standardised against a population culturally similar to that of the person being tested. Although IQ can change to some extent with increasing age, it is a surprisingly robust construct that is strongly predictive of achievement. IQ has a large inherited component, but environmental factors have a strong effect as well.
IQ measurement is mandatory in all cases in which ID is suspected. IQ should be measured using, if at all possible, widely accepted tests that have been standardized for the specific – or culturally similar – population. Widely used tests include the Wechsler Intelligence Scale for Children and the Stanford-Binet Intelligence Scales.
It is also useful to evaluate adaptive behaviour. To do that, professionals compare the functional abilities of a child to other children of similar age and education. There are many adaptive behaviour scales available, such as Vineland Adaptive Behavior Scales and Adaptive Behavior Assessment System-II, but an accurate assessment of children’s adaptive behaviour requires clinical judgment as well.
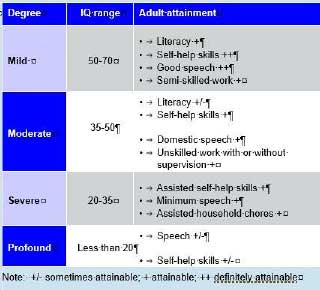
IQ scores more than two standard deviations below the mean, accompanied by adaptive impairments, are designated as intellectually disabled. Degrees of ID are designated Mild, Moderate, Severe or Profound when scores are three, four, five or more standard deviations below the mean. The following table gives a general indication of adaptive functioning at the different levels.
Management
In all cases of ID, the crux of treatment is early detection and early intervention. As no specific etiology can be found in up to 40% of cases and many known causes cannot be cured, in the majority of cases, the aim of treatment is not a “cure” but to minimize symptoms and disability through reducing risk (e.g., helping individuals to be safe at home or school), teaching life skills, improve life quality and support families and carers. Detailed goals and modalities of treatment for each individual will largely depend on the cause and severity of ID and comorbid conditions.
Challenging behaviours is a term used to describe comportment that interferes with the daily life of individuals with ID and their carers, reduce their quality of life and survival. These represent a wide range of problems that includes, among others, aggression, self-injury (such as head banging or ingestion or inhalation of foreign bodies), destroying objects, non-compliance, idiosyncratic habits (e.g., restricted range of foods), and socially inappropriate behaviour.
These problems frequently result in carers seeking medical help and can easily overwhelm families’ ability to cope with and care for these young people, often resulting in rejection or, in more severe cases, institutionalization.
As in non-ID individuals, challenging behaviours serve a function and they are maintained or reinforced if the person with ID is successful in altering their internal or external environment through their behaviour – such as by gaining attention, avoiding duties or demands, achieving access to preferred activities or objects or control over their own life, sensory feedback (eg. hand flapping, eye poking), and reduction of arousal and anxiety.
The current trend is to educate children with ID as far as possible in normal rather than special schools (inclusive education). This especially applies to those with milder forms of ID. However, there is limited evidence to compare the school experience of children with mild to moderate ID in
mainstream and segregated education.
Another approach is to conduct special classes for children with ID in normal schools (opportunity classes). More severely retarded children may benefit from special schools. Whatever the approach, children with ID need education – even more so than other children – to maximize their development and chances in life.
A major barrier to integration is the stigma that surrounds people with intellectual disability. The basis of this rejection of feared “Not-like-us” people is discussed in PE1d(ii). The extent of the rejection is easily seen in how past terminology of degrees of ID [idiot, moron, imbecile] has been incorporated as terms of abuse in everyday language. A significant part of management should include measures to reduce stigma and discrimination.
Reference
This paper has been largely taken from: Ke X, Liu J. Intellectual disability. In Rey JM (ed), IACAPAP e-Textbook of Child and Adolescent Mental Health. Geneva: International Association for Child and Adolescent Psychiatry and Allied Professions 2012.
AUTISM SPECTRUM DISORDERS
Autism spectrum disorder (ASD) refers to a neurodevelopmental condition defined by several behavioral features. The core clinical characteristics of ASD include impairments in two areas of functioning (social communication and social interaction), as well as restricted, repetitive patterns of behavior, interests or activities.
These symptoms are present in the early developmental period but may not be fully manifest until social demands exceed the child’s limited capacities or may be masked by learned strategies in later life. Despite its early unfolding, this condition is not necessarily diagnosed until a few years later.
There is a discussion in PE3a(ii) about Developmental Disorders including Autism Spectrum Disorders indicating that research has gradually changed the necessary and sufficient diagnostic criteria over the decades since initial description in scientific literature. The changed criteria have resulted in a greater acknowledged prevalence, about 1% of the child population.
This increased identification of this disorder, its emotional impact on families and the challenging financial demands associated with its treatment and support currently make ASD an important illness at the scientific, clinic and public health levels.
The current ASD category is characterized by:
The broad ranging patterns of functional impairments in ASD highlight the importance of careful clinical assessment of the young person’s strengths and limitations to arrive at optimal programs to maximise developmental progress in all domains.
Reference:
This paper has been largely taken from: Fuentes J, Bakare M, Munir K, Aguayo P, Gaddour N, Öner Ö. Autism spectrum disorder. In Rey JM (ed), IACAPAP e-Textbook of Child and Adolescent Mental Health. Geneva: International Association for Child and Adolescent Psychiatry and Allied Professions 2014.
Last updated 19/1/2022
POLICIES for Treatment of Mental Disorders. The project coordinator is Dr Allan Mawdsley. The version can be amended by consent. If you wish to contribute to the project, please email admin@mhyfvic.org
[6] Standard Treatment
a) Outpatient psychotherapies, medication and procedures
b) Inpatient psychotherapies, medication and procedures
c) Ancillary support services
[6 a ] Outpatient psychotherapies, medication and procedures
MHYFVic advocates that Specialist mental health services should offer a range of therapeutic programs for disabling mental health problems in the community. All disorders in childhood require wholistic management involving caregivers.
Service provision, clinical research and training should be integrated in the Tier Three facilities, with the practice guidelines published by those services implemented at all levels of their service delivery facilities. The baseline standard of case assessment required is that outlined in PE4 (and PE2a(i) for infant mental health)
POL6a (viii) Developmental Disorders and Intellectual Disability
MHYFVic advocates that Specialist mental health services should offer multidisciplinary assessment and treatment programs for children with intellectual disability and developmental disorders including autism spectrum disorders. Such services would include ongoing collaboration with families and consultative support to other agencies involved in the management plan. It would also include components for management of challenging behaviours.
Last updated 19/1/2022
PROJECT EVIDENCE for Treatment of Mental Disorders. The project coordinator is Dr Allan Mawdsley. The version can be amended by consent. If you wish to contribute to the project, please email admin@mhyfvic.org
[6] Standard Treatment
a) Outpatient psychotherapies, medication and procedures
b) Inpatient psychotherapies, medication and procedures
c) Ancillary support services
[6 a ] Outpatient psychotherapies, medication and procedures
Specialist mental health services should offer a range of therapeutic programs for disabling mental health problems in the community. Service provision, clinical research and training are closely linked in the Tier Three facilities but the practice guidelines published by those services should be implemented at all levels of their service delivery facilities.
These are grouped under nine headings: (i) organic brain disorders, (ii) substance abuse disorders, (iii) psychotic disorders, (iv) mood disorders, (v) anxiety disorders, including stress-related, somatoform and obsessive-compulsive disorders, (vi) physiological disorders, including eating, sleeping and sexual, (vii) personality disorders, (viii) intellectual disability and developmental disorders including autism spectrum disorders, (ix) behavioural and relationship disorders of childhood.
All disorders in childhood require wholistic management involving caregivers. See PE4 for a general outline of case identification and assessment and PE2a(i) for infant mental health. See PE6a(ix) for a general outline of case management for young people.
BP6a (viii) Developmental Disorders and Intellectual Disability
The general principles of clinical assessment and case planning mentioned in the preceding paragraph are modified in the case of developmental disorders and intellectual disability because of the diverse range of specialist skills required for adequate management and the expectation of long-term shared involvement.
The additional principle is that management should be through a specialist multi-disciplinary team with capacity for continuity of care and ongoing partnership with the young person’s family. The multi-disciplinary team should include contributions of specialists in all the relevant fields of the child’s impairments (eg. Psychology, Speech pathology, Occupational therapy, Special education, etc).
INTELLECTUAL DISABILITY
The term ‘intellectual disability’ (ID) is defined as “a condition of arrested or incomplete development of the mind, which is especially characterized by impairment of skills manifested during the developmental period, which contribute to the overall level of intelligence, i.e., cognitive, language, motor, and social abilities.” (World Health Organization, WHO, 1992).
The etiology of ID is heterogeneous. It is an important part of assessment to ascertain the etiology. The immediate reason is to ensure that it is not a treatable ongoing cause (such as thyroid deficiency) that will further worsen if untreated. This generally requires a specialist paediatric medical assessment process.
On most occasions the developmental damage has been done and will remain unchanged and not specifically treatable. However, the impairment that produces a functional disability will result in a degree of handicap that is variable, depending upon management. It is a crucial part of assessment and management to minimise handicap and optimise developmental progress.
Regardless of whether etiology can be treated, or even ascertained, a further important reason for diagnostic assessment is to add to the knowledge base about intellectual disability by which prevention and possible future treatment approaches may be promoted.
IQ measurement is mandatory in all cases in which ID is suspected. IQ should be measured using, if at all possible, widely accepted tests that have been standardized for the specific – or culturally similar – population. Widely used tests include the Wechsler Intelligence Scale for Children and the Stanford-Binet Intelligence Scales.
It is also useful to evaluate adaptive behaviour. To do that, professionals compare the functional abilities of a child to other children of similar age and education. There are many adaptive behaviour scales available, such as Vineland Adaptive Behavior Scales and Adaptive Behavior Assessment System-II, but an accurate assessment of children’s adaptive behaviour requires clinical judgment as well.
Management
In all cases of ID, the crux of treatment is early detection and early intervention. The aim of treatment is to minimize symptoms and disability through reducing risk (e.g., helping individuals to be safe at home or school), teaching life skills, improve life quality and support families and carers. Detailed goals and modalities of treatment for each individual will largely depend on the cause and severity of ID and comorbid conditions.
The current trend is to educate children with ID as far as possible in normal rather than special schools (inclusive education). Whatever the approach, children with ID need education – even more so than other children – to maximize their development and chances in life.
Challenging behaviours represent a wide range of problems that includes, among others, aggression, self-injury (such as head banging or ingestion or inhalation of foreign bodies), destroying objects, non-compliance, idiosyncratic habits (e.g., restricted range of foods), and socially inappropriate behaviour.
These problems require specialist treatment programs within the educational and home settings as part of the case management plan. A further significant part of management should include measures to reduce stigma and discrimination.
AUTISM SPECTRUM DISORDERS
Autism spectrum disorder (ASD) refers to a neurodevelopmental condition defined by several behavioral features. The core clinical characteristics of ASD include impairments in two areas of functioning (social communication and social interaction), as well as restricted, repetitive patterns of behavior, interests or activities.
These symptoms are present in the early developmental period but may not be fully manifest until social demands exceed the child’s limited capacities or may be masked by learned strategies in later life. Despite its early unfolding, this condition is not necessarily diagnosed until a few years later.
In addition to the notes in PE6a(viii) there is a discussion in PE3a(ii) about Developmental Disorders including Autism Spectrum Disorders indicating that research has gradually changed the necessary and sufficient diagnostic criteria over the decades since initial description in scientific literature.
The changed criteria have resulted in a greater acknowledged prevalence, about 1% of the child population. This increased identification of this disorder, its emotional impact on families and the challenging financial demands associated with its treatment and support currently make ASD an important illness at the scientific, clinic and public health levels.
The broad ranging patterns of functional impairments in ASD highlight the importance of careful clinical assessment by a multi-disciplinary team of the young person’s strengths and limitations to arrive at optimal programs to maximise developmental progress in all domains.
Last updated 19/1/2022
We welcome discussion about any of the topics in our Roadmap epecially any wish to develop the information or policies.
Please send your comments by email to admin@mhyfvic.org
Speak about issues that concern you such as gaps in services, things that shouldn’t have happened, or things that ought to happen but haven’t; to make a better quality of service…….
Help achieve better access to services & better co-ordination between services together we can…….

Mental Health for the Young & their Families in Victoria is a collaborative partnership between mental health & other health professionals, service users & the general public.
MHYFVic
PO Box 206,
Parkville, Vic 3052

Please fill in the details below and agree to the conditions to apply for MHYFVic membership.