
Mental Health for the Young & their Families in Victoria is a collaborative partnership between mental health & other health professionals, service users & the general public.
Mailing Address
MHYFVic
PO Box 206,
Parkville, Vic 3052
PROJECT EVIDENCE for Treatment of Mental Disorders. The project coordinator is Dr Allan Mawdsley. The version can be amended by consent. If you wish to contribute to the project, please email admin@mhyfvic.org
[5] Early Treatment
a) Universal Health, Welfare and Education agencies in the community. [Tier 1]
b) Private practitioners and Community Mental Health services [Tier 2]
c) Specialist Mental Health Services [Tier 3]
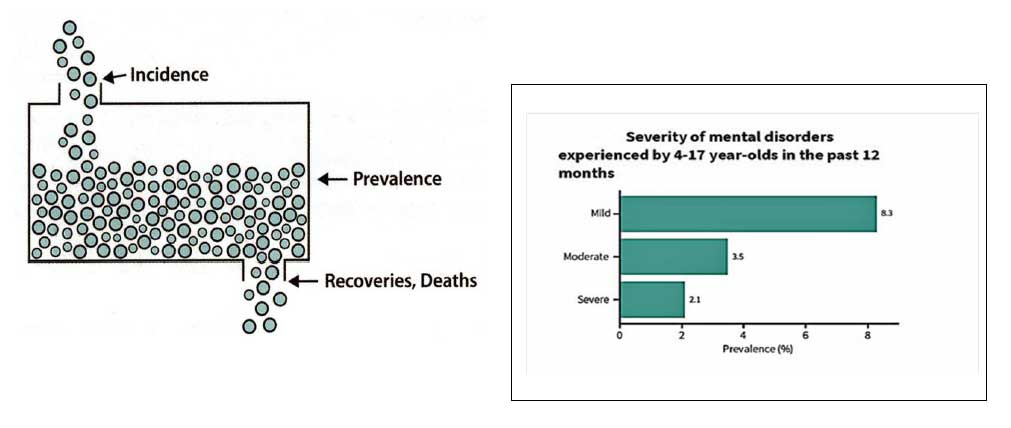
At any time about 15-20% of the population has some degree of mental disturbance. Most are of mild degree and some get better without formal treatment. However, some get worse and will need extensive treatment who would have been better treated early rather than later. The ideal system allows early assessment and management, with triage of those which require more specialised treatment. At present, only about 5% of cases receive formal treatment.
The majority of cases are first encountered at universal health, welfare and education services in the community and it is therefore important to have a system that is able to respond appropriately to the needs.
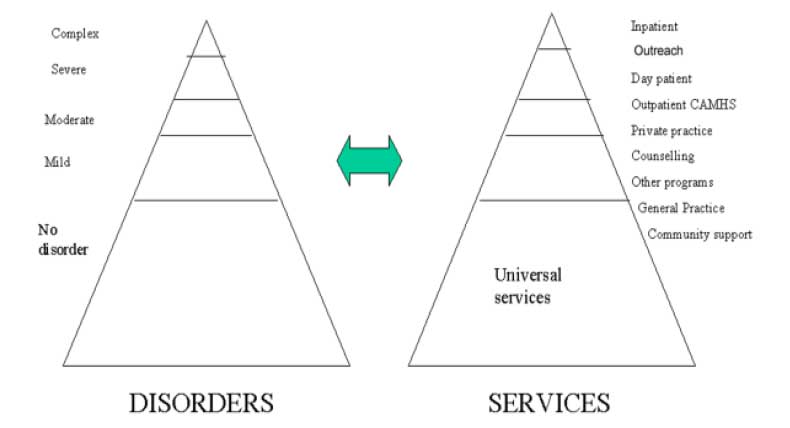
The twin pyramids diagram represents the distribution of mental disorders in the community and the range of services that respond to them. There is a rough correspondence between the strata of each pyramid, with severe and complex cases being seen by hospital services whilst milder cases are seen by community-based agencies. This is generally appropriate, but also indicates how systemic difficulties occur when there are major barriers to collaboration between service delivery agencies in each stratum.
Each stratum has various silos of funding and accountability, with minimal incentive to assist other agencies and maximal incentive to designate problems as the responsibility of other agencies. This is primarily because, without coordination of the whole system, each component agency sets its own inclusion criteria, key performance indicators and constraints on funding allocation, without regard to the unmet needs. Improved collaboration, even within existing resource allocation, would result in improved services. Response with additional funding targeted at case-sharing would be even greater.
What we need is a system that:
The current patchwork system cannot provide these needs and a new system is required. The new system should be based upon a restructuring of agency responsibilities within existing service tiers.
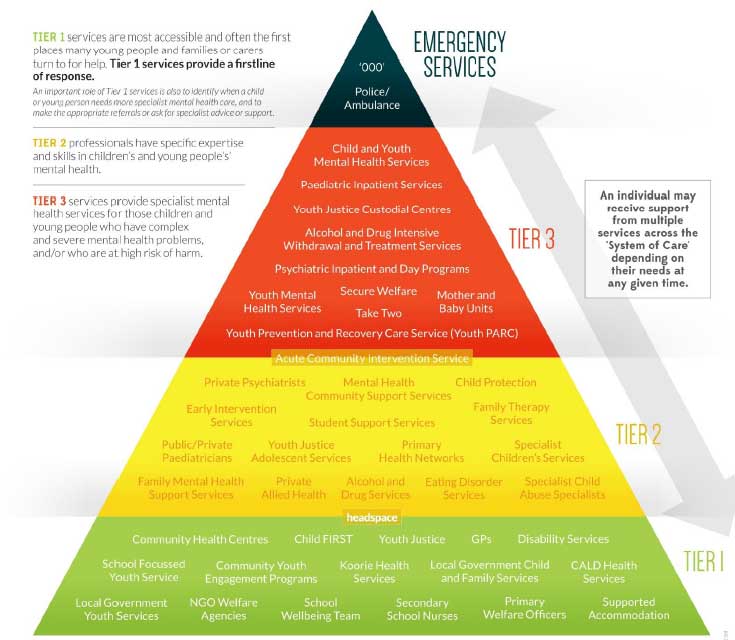
The National Mental Health Working Group’s report “Responding to the Mental Health Needs of Young People ln Australia” describes the service system using a ‘tiers of care’ approach to meet the needs of young people with mental health issues (Department of Health and Ageing 2004).
The three tiers are:
Tier 1 services are usually the first point of contact when problems start and provide the first line of response for most young people. Importantly, although Tier 1 services generally have no formal mental health training, they identify when a person needs more specialist intervention and supports the person to seek help or makes the appropriate referral.
These services may include:
Tier 2 services are health professionals such as (but not limited to) private psychologists, social workers, some GPs who have some mental health training who tend to see young people who have moderate to severe disorders or those at higher risk of developing a mental health disorder. These interventions are generally provided in the community and school settings.
Tier 3 services provide multidisciplinary intensive levels of care, crisis response and assertive outreach and inpatient services to young people who are difficult to engage and have complex needs. Tier 3 includes services provided by the non-government mental health sector.
ln order to maximise the resilience, capacities and positive mental health of young people, a child and youth mental health system of care is required that incorporates and supports the continuum of ‘services’ at an appropriate level and in a coordinated and integrated way.
The following diagram from the South Australian Health Department website shows the range of child, youth and family services in the tiers of the MHYFVic-style service pyramid.
Tier Three services at present are mainly devoted to management of seriously mentally ill patients in designated mental health facilities. They undertake some outreach service but generally have significant barriers to intake of new cases. It would be better for the community if the expertise of this tier was made available to tier two for the management of its less severe cases.
Tier Three specialist mental health services should provide:
There should be no direct referral to Tier Three units. All referrals for specialist mental health services should come through the intake service at Community Health Centres (Tier Two), staffed by Outreach Workers from the Tier Three services. In this way the specialist services can maintain control of their admissions whilst simultaneously ensuring that cases not admitted to the specialist units are provided with appropriate alternative support. This may be programs within the Community Health Centres or other services such as private practitioners, but no cases would be left unserviced.
The same Tier Three services outreach staff acting as intake workers at Community Health Centres would also provide the same service at Emergency Departments at General Hospitals and by outreach Community Assessment and Treatment Teams responding to emergency calls in the community (such as Involuntary Admission recommendations from GPs). Tier Three services are considered in more detail in Project Evidence paper PE 5 c.
Tier Two services should be the default outpatient treatment provider for cases that are too difficult for Tier One and do not require the hospital care of Tier Three, also for coordinated multidisciplinary assessments.
Tier Two Community Health services should provide:
No person should be refused access to assessment, and all persons should be case-managed in Tier Two, notwithstanding that components of service may also be provided by Tier Three as necessary. This does not happen adequately at present, mainly because of different centres of accountability and funding, which are not required to collaborate, but could do so if required.
General Medical Practitioners and other allied health professionals funded through Medicare could deal with a high proportion of cases. The psychological treatment programs of Community Health Centres could deal with self-referred clients or those referred by GPs because of chronicity or difficulty too great for primary care. Specialist mental health (Tier Three) workers should provide sessional input for the Community Health workers to ensure that the treatment programs can cater for the needs of the clientele or facilitate transition to Tier Three services if necessary.
Tier Two services are considered in more detail in Project Evidence paper PE 5 b.
Tier One services are the universal health, welfare and educational services in the community. They are the focus of this paper:
[5 a ] Universal Health, Welfare and Education agencies in the community.
Universal services such as Maternal and Child Health Centres, Municipal Social Work Departments, Youth Workers, School Counsellors, non-government agencies and various support services are used by many of the population.
Persons who have not perceived themselves as having mental disorders may be clients of such Tier One services. Tier One workers need a basic understanding of mental health issues. When alerted to symptoms potentially indicative of mental disorder it is important for Tier One workers to respond appropriately.
Appraisal of the nature of the disorder and its attendant risks, deciding upon the management pathway most likely to help, and the successful engagement of clients with that pathway, are the primary tasks. These tasks depend upon a positive relationship with the client.
If the Tier One worker has an established positive relationship, ongoing management may be more successful than an attempt at referral to a specialist service that fails to engage. There are often resistances in clients and agencies that prevent engagement, and a failed engagement can result in the loss of the former support as well as the suggested one.
This is particularly problematic when there are multiple issues prompting fragmentation of care. For example, families in which there is alcohol abuse, family violence, marital and child behaviour problems. A worker who is engaged with the family, even when less skilled in the various issues confronting them, may achieve better results than experts who cannot engage.
The Tier One worker in such circumstances needs support at several levels. The foundation level is a basic training about Mental Health problems; this is described in Project Evidence PE 9 c. The next level is case discussion with a mental health specialist, referred to as ‘Secondary Consultation’, described in Project Evidence PE 9 b. If such discussion reaches the conclusion that referral to more specialised services is required, support is needed in liaising between clients and services and successfully arranging the transition.
If the clients refuse such referral there remains a possibility for conjoint meeting with clients and mental health specialist, referred to as ‘Primary Consultation’, described in Project Evidence PE 9 b, with a view to maintaining case management under supervision.
In the ordinary course of events it should be possible for Tier One workers to arrange transition to Tier Two specialist services. Private practice specialists generally make their own transition arrangements. What is needed for future development of this proposed collaborative network, is for Community Health Services to have a readily responsive Intake and Short-term management capability that will take responsibility for assessment and care of all such referrals. The recommended method is described in Project Evidence PE 5 b.
Last Updated 24 April 2020
POLICIES for Treatment of Mental Disorders
[5] Early Treatment
a) Universal Health, Welfare and Education agencies in the community. [Tier 1]
b) Private practitioners and Community Mental Health services [Tier 2]
c) Specialist Mental Health Services [Tier 3]
[5 a ] Universal Health, Welfare and Education agencies in the community.
MHYFVic advocates that the State Government develops a collaborative project between its Health, Welfare, and Education Departments and Local Government for the commencement of a network of Child & Family Centres similar to the Tasmanian CFC model. (See “Overview of Child and Family Centres” pdf downloadable from Hot Issues in Mental Health page of MHYFVic website.)
MHYFVic advocates that the age range for CFC service is extended to adolescence within Community Health Centres.
MHYFVic advocates that mental health specialist consultancy is provided to CFC programs through the outreach component of service described in Project Evidence PE5c.
Last updated 2 April 2020
BEST PRACTICE MODELS for Treatment of Mental Disorders
[5] Early Treatment
a) Universal Health, Welfare and Educational agencies in the community [Tier 1]
b) Private practitioners and Community Mental Health services [Tier 2]
c) Specialist Mental Health services [Tier 3]
Mental health disorders occur throughout the community at various levels of severity. At present, diverse private and public sector agencies respond to aspects of mental health need in an un-coordinated manner. MHYFVic proposes a coordinating framework to ensure that appropriate care is delivered. This is described in Project Evidence PE 5 a.
[5 a ] Universal Health, Welfare and Educational agencies
The Child and Family Centres developed by the Tasmanian government in 2010, for children in the 0-5 age range, offer the best practice model for services everywhere, although it would be desirable for the model to be extended to higher age ranges. Their operation is explained in the document “An Overview of Child and Family Centres” which is downloadable from the MHYFVic website in the “Hot Issues in Mental Health” page.
The rationale for CFC is in response to the steadily growing body of research evidence from around the world about the critical importance of the early years and the need for a radical shift in the way services are delivered to children and families. It becomes increasingly difficult to change trajectories of children as they grow older. Investments in early childhood services are shown to be cost effective, yielding long term benefits to children and to society. The earlier the services are provided the greater the economic return.
In order to deliver maximum community benefit, CFCs should provide a truly integrated service delivery model. The co-location of services for children and families should be situated within an overarching vision and set of goals that sees a fundamental re-engineering of the full range of services currently delivered by Government agencies, particularly those provided by the Department of Health and Human Services and the Department of Education, as opposed to simply moving services to a single site. The document identifies the following features:
All Child and Family Centres will:
Child and Family Centres (CFCs) are:
Child and Family Centres have…
Child and Family Centres are not:
All services provided from a CFC will:
[1] Any reference to ‘parents’ in this document refers also to carers, grandparents and legal guardians, however they are constituted within the community
If the above model was provided, incorporating access to community health programs, child care centres and kindergartens in all municipalities, and including the intake/ short-term assessment and
treatment components described in PE5a, this would give the ideal community coverage and accessibility for mental health services.
Last updated 2 April 2020
We welcome discussion about any of the topics in our Roadmap epecially any wish to develop the information or policies.
Please send your comments by email to admin@mhyfvic.org
Speak about issues that concern you such as gaps in services, things that shouldn’t have happened, or things that ought to happen but haven’t; to make a better quality of service…….
Help achieve better access to services & better co-ordination between services together we can…….

Mental Health for the Young & their Families in Victoria is a collaborative partnership between mental health & other health professionals, service users & the general public.
MHYFVic
PO Box 206,
Parkville, Vic 3052

Please fill in the details below and agree to the conditions to apply for MHYFVic membership.